In Vitro Fertilization (IVF) is a ray of hope for many people worldwide who dream of having a child. As a complex yet fascinating assisted reproductive technology, IVF has been breaking barriers in infertility treatment, offering a chance at parenthood to those who might otherwise have remained childless.
Motivated by a combination of compassion and science, our IVF experts work hand-in-hand with each patient, turning their dream into a realistic plan.
Understanding that the process can be emotionally overwhelming, we’re committed to supporting our patients at every step.
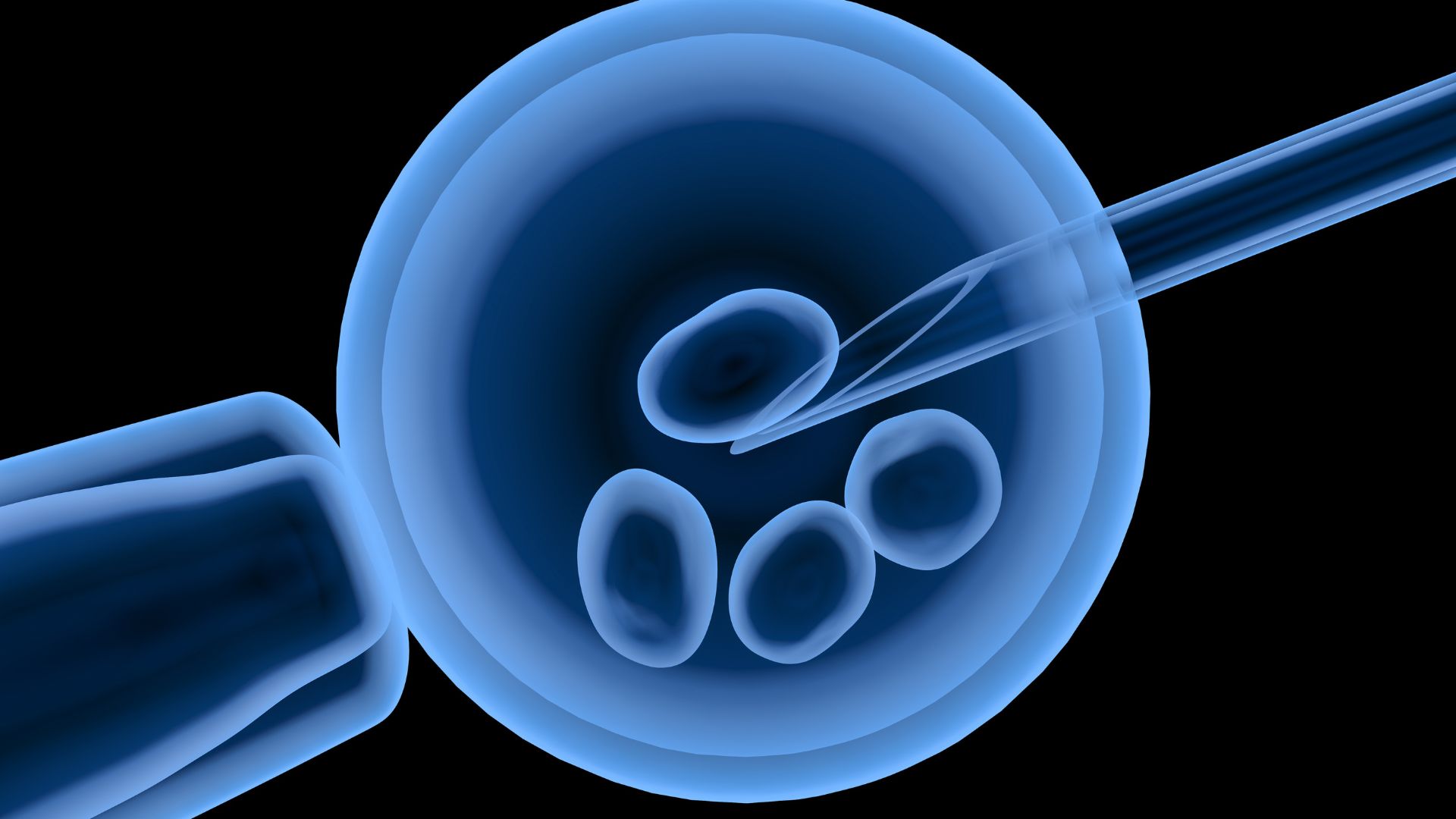
IVF involves the fertilization of an egg outside the body. Eggs are retrieved from the ovaries and fertilized with sperm in a specialized laboratory.
The resulting embryos are then transferred into the woman’s uterus, where one or more may implant and develop into a pregnancy.
But before diving into what to expect during this complex and intricate process, it is essential to understand the context—the reasons why IVF is chosen as a fertility treatment.
While IVF can be beneficial for those with a vast array of infertility issues, from fallopian tube damage to reduced ovarian reserve to unexplained infertility, it’s not always the first line of treatment.
Taking the leap towards IVF often involves a cocktail of emotions—fear of the unknown mingling with the exhilaration of possibility.
We’ve compiled this comprehensive guide to answer your common IVF questions and help you navigate through the intricate labyrinth of this medical marvel.
It’s important to remember that each individual’s path is uniquely crafted to their specific medical landscape, and this guide provides a general understanding of the journey.
In the upcoming sections, we’ll unravel the details of IVF’s preparation phase, the intimidating labyrinth of the IVF cycle—from ovarian stimulation to egg retrieval investigating the egg/oocyte retrieval process—and the final steps of embryo transfer and implantation.
Throughout this narrative, we’ll keep in mind the emotional landscape of our readers because empathy and understanding are just as important as science and success rates.
The decision to start your journey towards IVF is not simple and often comes after several other treatments have been unsuccessful.
If you’re considering this step, consult with our fertility specialists to have a discussion why and when to do IVF, adjusting your trajectory as needed based on individual circumstances and medical advice.
As we delve deeper into the subject, we’ll also touch on IVF’s potential side effects and pick apart some of the techniques involved in the process, like Intracytoplasmic Sperm Injection (ICSI).
Preparing for Your IVF Journey
Embarking on the IVF journey presents a mix of hope and uncertainty. Before treatment begins, several preparatory steps must be taken to pave the way for the best possible outcome.
Initial Consultation: Laying the Groundwork for Success
The first beacon on the IVF pathway is the initial consultation with a fertility specialist. This meeting is much more than a routine doctor’s appointment; it’s the foundation upon which your entire treatment plan is built.
Your doctor will review your complete medical history and discuss previous attempts at pregnancy, lifestyle factors, and any fertility treatments tried in the past.
Both partners will undergo tests to assess overall health and fertility status. This step is crucial, as it allows your care team to tailor the IVF process to your individual needs, enhancing your chances of success.
Pretreatment Medications: Priming for Potential
In preparation for the IVF cycle, your doctor may prescribe a specific protocol, including birth control pills or other hormone treatments.
It might seem counterintuitive to take birth control when your goal is to become pregnant, but it’s a strategic move.
These medications help synchronize your cycle, quieting the ovaries and ensuring that they respond optimally to the forthcoming fertility drugs that stimulate egg production. This precise timing and control are essential for maximizing the efficiency of the process.
The IVF Cycle Explained
Once preparation is complete, the IVF cycle begins. The cycle can be emotionally and physically challenging, but understanding each step can offer peace of mind and clarity as you navigate these uncharted waters.
Step 1: Ovarian Stimulation: The Quest for Multiple Eggs
The cornerstone of the IVF cycle is stimulating the ovaries to produce multiple eggs. In a typical menstrual cycle, only one egg is released; however, IVF aims for multiple eggs to increase the chances that a viable embryo can be transferred back to the uterus.
To achieve this, you’ll administer daily injections of FSH, alongside other possible medications, for about two weeks.
Regular monitoring through ultrasounds and blood tests allows your care team to observe the development of the follicles (fluid-filled sacs that contain the eggs) and adjust medication dosages to optimize egg maturation.
Step 2: Egg Retrieval: Securing the Precious Cargo
Egg retrieval is a pivotal event. Following the ovarian stimulation, you’re given a ‘trigger shot,’ which induces the final maturation of the eggs.
The retrieval procedure itself typically takes about 20-30 minutes, during which eggs are aspirated from the follicles under sedation.
It’s a low-risk procedure, but, as with any medical intervention, there is a small chance of complications, which your healthcare team is prepared to manage.
Step 3: Fertilization: The Union of Egg and Sperm
After the eggs are harvested, they are taken to the lab, where the magic of fertilization occurs. Your partner’s sperm or donor sperm is prepared and introduced to the eggs.
Alternatively, if there are concerns about sperm quality or previous fertilization issues, ICSI may be employed.
This technique involves injecting a single healthy sperm directly into an egg. Successful fertilization marks the beginning of an embryo’s development.
The IVF Cycle Continues: Embryo Development to Transfer
Once fertilization has occurred, the fertilized eggs, now embryos, are nurtured in the controlled environment of the laboratory.
This stage is critical as each embryo embarks on a journey from a single cell to a complex structure capable of implanting in the uterine lining.
Step 4: Embryo Development: The Laboratory Watch
The embryos are carefully monitored as they divide and grow. Typically, after 3 to 5 days of development, they reach a stage called the blastocyst, indicating they are ready for transfer or freezing.
Advanced genetic screening may be offered at this point to identify embryos with the best chance of success, reducing the risk of genetic abnormalities.
Step 5: Embryo Transfer: The Pinnacle of the IVF Process
The transfer of embryos is a moment filled with anticipation. It’s a painless procedure requiring no sedation. One or more embryos are placed inside the uterus using a thin catheter.
While the decision on the number of embryos to transfer is complex, it involves considering many factors to balance the chance of success against the risk of multiple pregnancies.
After the transfer, patients often resume normal activities, with a recommendation to avoid strenuous activities for a short period.
Emotional Considerations and the Wait
The period following the embryo transfer, commonly known as the two-week wait, can be one of the most emotionally taxing times for patients. It’s a period full of hope and anxiety as you await the first signs of pregnancy.
The Pregnancy Test and Beyond
Approximately two weeks after the transfer, a blood test will confirm if implantation has occurred. If the test is positive, congratulations are in order; this is a significant milestone.
However, it’s only the beginning of the pregnancy journey, requiring ongoing medical support.
Subsequent Steps: Freezing Embryos and Future Cycles
If there are more viable embryos than were used in the transfer, the decision to freeze them can be a significant advantage for future fertility plans.
Cryopreserved embryos greatly reduce the need for repeated ovarian stimulation and egg retrieval, simplifying subsequent attempts at IVF.
Understanding Success Rates and Side Effects in IVF
As we navigate the final bends of our IVF journey, let’s address two critical areas: the potential side effects of IVF and the success rates that provide hopeful parents with essential data.
Side Effects: Navigating the Physical Impact
IVF medications and procedures come with an array of possible side effects. While most are mild and manageable, it’s crucial to be informed.
Ovarian stimulation can lead to feelings of fullness or bloating, mood swings, or headaches. In rare cases, Ovarian Hyperstimulation Syndrome (OHSS), a more serious condition, may occur.
Following egg retrieval, expect some bloating and a degree of discomfort, which typically resolves quickly. The fertility care team is always on standby to offer advice and support for managing these side effects.
IVF Success Rates: Numbers Tell a Story
Understanding success rates is essential, as they help set realistic expectations.
According to the Society for Assisted Reproductive Technology (SART), the success rates for IVF vary significantly by age, with younger women generally experiencing higher success rates.
It’s important to discuss these statistics with your fertility specialist to understand how they apply to your individual case.
Conclusion: Personalized Guidance on the Path to Parenthood
Each couple’s fertility journey is nuanced, shaped by personal history, health, and even the unpredictability of biology itself.
While this article aims to provide understanding and support, it’s vital to remember the importance of personalized medical advice.
With assisted reproductive technologies like IVF, countless individuals and couples have realized their dreams of parenthood.
By arming yourself with knowledge and choosing a team of compassionate specialists, the journey can become less daunting and more hopeful.






